Accurate and widespread testing is crucial to managing the coronavirus pandemic, yet many people don’t have access to tests. To get tested for COVID-19, the disease caused by the virus SARS-CoV-2, patients typically must visit designated testing sites. But a new research project could lead to an affordable, at-home test that offers rapid detection.
Researchers from the University of Chicago’s Pritzker School of Molecular Engineering (PME) and Department of Pathology were awarded a Big Ideas Generator (BIG) grant to develop a handheld COVID-19 testing device that provides results in five minutes.
BIG, which awarded the research team $80,000 in direct cost funding, funds early-stage research projects at UChicago that have the potential to grow into novel and robust areas of research.
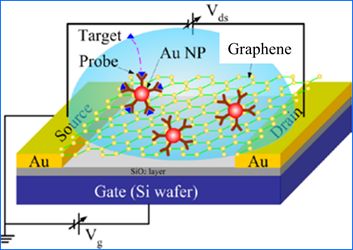
With this funding, Pritzker Molecular Engineering researchers Jun Huang and Junhong Chen, their lab groups, and Kathleen Beavis of the Department of Pathology will come together to create a detection device that uses field-effect transistor technology to enable rapid diagnosis of COVID-19 at home and point-of-care.
Affordable, at-home testing
Haihui Pu, a staff scientist in the Junhong Chen research group, said a home testing kit could provide peace of mind to individuals who might be concerned about the risk of exposure to the coronavirus at a testing site, as well as rapid results to those who might face a long wait or may not qualify based on their symptoms.

“Home testing offers the opportunity to carry out the self-diagnosis even with very mild symptoms or in the asymptomatic condition,” Pu said. “In addition, it is affordable at about $10 per test.” An affordable price point is critical for under-resourced and underserved populations to access the technology, he added.
To meet the high demand for testing, the researchers plan to use cost-effective technology that is sensitive, precise, reliable, and high-throughput. Nicholas Ankenbruck, a postdoctoral researcher in the Huang lab, said creating an accurate test will require the use of purified biological materials for extensive evaluation before moving on to actual patient samples.
“This new funding enables us to purchase all the necessary resources in order to fine-tune and calibrate the device to ensure it is ready for patient use,” he said.
Detecting both the virus and antibodies
The researchers plan to create a handheld device programmed with step-by-step prompts on the LCD screen, allowing for easy use without any prior training. The device would use various specimens from patients (e.g., nasal and sputum samples) to test for both infection and antibodies.

“The existing technologies only allow for diagnosis against COVID-19 by separately detecting the presence of virus and antibodies, which also require professional training for operation and take hours to deliver the results,” said Pu.
The research team’s device, however, will detect viral particles and antibodies simultaneously.
“In order to do this,” Ankenbruck explained, “we immobilize probes specific to the virus or antibodies on the surface of the device, and then monitor changes in electrical measurements in the presence of a sample.”
This combined detection is important, Ankenbruck said, because it can hint at the stage of viral infection or indicate whether the individual is unable to produce antibodies to fight the infection. In other words, people could use the testing device to track the progression of the disease from home.
For example, if a user takes the test when they first have symptoms, it may detect the virus but no antibodies. A week later, that user may detect both the virus and antibodies, suggesting their body is starting to fight off the infection. And if a user is not getting better within a reasonable time frame, they will know it's time to call the doctor for intervention.
A collaborative approach
Each member of the research team brings specific expertise to the project. Junhong Chen, also lead water strategist at Argonne National Laboratory, has extensive experience in nanomaterials and nanodevices. His group will provide the central sensing platform for the device. Jun Huang and his lab group focus on immunology. They will develop a pseudovirus, or synthetic virus, to enable optimization of the device.